Craniotomy
What is a craniotomy?
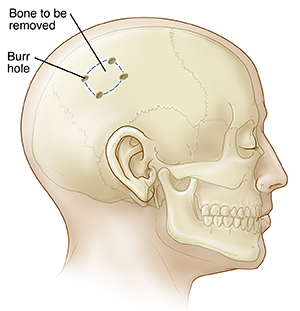
A craniotomy is the surgical removal of part of the bone from the skull to expose the brain for surgery. The surgeon uses special tools to remove the section of bone (the bone flap ). After the brain surgery, the surgeon replaces the bone flap and attaches it to the surrounding bone with small titanium plates and screws. If part of the skull bone is removed and not replaced right away, it is called craniectomy. This is done if brain swelling is likely after brain surgery. Or if the skull bone flap can't be replaced for other reasons. After a few weeks to months, you may have a follow-up surgery called a cranioplasty. During a cranioplasty, the missing piece of skull will be replaced with your original bone, a metal plate, or a synthetic material.
.
For some craniotomy procedures, healthcare providers use MRI or CT scans. Imaging helps guide the healthcare provider to the exact place in the brain that is to be treated. It is called image-guided craniotomy or stereotactic craniotomy when computers and imaging are combined to make 3-D pictures.
A craniotomy can be done with various tools that help the surgeon see the area of the brain. These include loupes, a microscope, high-definition cameras, or an endoscope. A craniotomy with an endoscope involves putting a lighted small tube attached to a camera into the brain through a small hole in the skull.
Why might I need a craniotomy?
Healthcare providers may do a craniotomy for a variety of reasons, including to:
-
Diagnose, remove, or treat brain tumors
-
Clip or repair an aneurysm
-
Remove blood or blood clots from a leaking blood vessel
-
Remove an arteriovenous malformation. This is an abnormal mass of blood vessels.
-
Drain an infected pus-filled pocket (abscess)
-
Repair skull fractures
-
Repair a tear in the membrane lining the brain (dura mater)
-
Relieve pressure within the brain (intracranial pressure) by removing damaged or swollen areas of the brain that may be caused by traumatic injury or stroke
-
Treat epilepsy. This is a neurological condition involving the brain that makes people more likely to have seizures.
-
Implant stimulator devices to treat movement disorders. These include Parkinson disease or a type of movement disorder called dystonia.
-
Treat hydrocephalus
There may be other reasons for your healthcare provider to advise a craniotomy.
What are the risks of a craniotomy?
Any surgery can have complications. Brain surgery risk is tied to the specific place in the brain that the surgery will affect. For example, if the area of the brain that controls speech is operated on, then speech may be affected. Some more general complications include:
-
Infection
-
Bleeding
-
Blood clot
-
Infection of the lungs (pneumonia)
-
Unstable blood pressure
-
Seizures
-
Muscle weakness
-
Brain swelling
-
Leakage of the fluid that surrounds and cushions the brain (cerebrospinal fluid or CSF)
-
Risks of general anesthesia
The following complications are rare and generally relate to certain places in the brain:
There may be other risks depending on your specific health condition. Discuss any concerns with your healthcare provider before the procedure.
How do I get ready for a craniotomy?
In many cases, a craniotomy is done urgently. If your craniotomy is planned, check with your healthcare provider about what to do to get ready for the procedure. Below is a list of common steps that you may be asked to do.
-
You will be asked to sign a consent form that gives permission to do the surgery. You will need to sign a separate form for getting anesthesia. Read the form carefully and ask questions if something is not clear.
-
In addition to a complete health history, your healthcare provider will do a physical exam. This is to make sure you are in otherwise good health before you have the surgery. You may also need blood tests and other diagnostic tests.
-
You will have a neurological exam before surgery that will be compared with one done after surgery.
-
You will be asked to fast before the procedure, generally after midnight.
-
If you are pregnant or think you might be, tell your healthcare provider.
-
Tell your healthcare provider if you are sensitive to or are allergic to any medicine, latex, tape, and anesthetic medicines, either local or general.
-
Tell your healthcare provider of all prescribed medicines, over-the-counter medicines, and herbal supplements that you are taking.
-
Tell your healthcare provider if you have a history of bleeding disorders. Or if you are taking any blood-thinning medicine, aspirin, or other medicine that affects blood clotting. You may need to stop these before the procedure.
-
If you smoke, you should stop smoking as soon as possible before the procedure to improve your chances for a successful recovery.
-
You may be asked to wash your hair with a special antiseptic shampoo the night before the surgery.
-
You may get medicine (sedative) before the procedure to help you relax.
-
Based on your condition, your healthcare provider may request other specific preparation.
What happens during a craniotomy?
A craniotomy generally needs a hospital stay of 3 to 7 days or more. This depends on your condition. You may also go to a rehabilitation (rehab) unit for several days after your hospital stay. Procedures may vary depending on your condition and your healthcare provider's practices.
Generally, a craniotomy follows this process:
-
You will take off any clothing, jewelry, or other objects that may interfere with the procedure and put on a hospital gown.
-
An IV (intravenous) line will be put in your arm or hand so you can get fluids and medicines.
-
A urinary tube (catheter) will be put in your bladder to drain your urine.
-
You will be placed on the operating table to give the surgeon the best access to the side of the brain to be operated on.
-
The anesthesiologist will watch your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
-
Staff may or may not shave your head. The skin over the surgical site will be cleaned with an antiseptic solution.
-
Your head will rest on a cushion or may be held in place by a device. The device will be removed at the end of the surgery.
-
The surgeon may use different types of cuts (incisions), depending on the affected area of the brain. If an endoscope is used, the incisions may be smaller.
-
The surgeon will pull up your scalp and may use skin clips to control bleeding.
-
The surgeon may use a medical drill to make burr holes in the skull. They may use a special saw to carefully cut the bone.
-
The bone flap will be removed and may be saved.
-
The surgeon will separate the thick outer covering of the brain directly underneath the bone (dura mater) from the bone and carefully cut it open to expose the brain.
Extra fluid will be allowed to flow out of the brain, if needed. Your surgeon may use microsurgical tools, such as a surgical microscope to magnify the area being treated. This gives the surgeon a better view of the brain
What happens after a craniotomy?
In the hospital
Right after the procedure, you will be taken to a recovery room to be closely watched. This is before being taken to a regular room or to the intensive care unit (ICU). In some cases, you may be taken directly to the ICU from the operating room. In the ICU, you may be given medicine to decrease the brain swelling.
You may have in place a brain intracranial pressure (ICP) device to keep track of the pressure in your brain. Or you may have an external ventricular drain to remove extra cerebrospinal fluid (CSF). These devices are often removed after a few days.
You may have a few catheters to get or drain fluid, or to keep track of your blood pressure.
Your recovery will vary depending on the type of procedure done and the type of anesthesia you had. Once your blood pressure, pulse, and breathing are stable and you are alert, you may be taken to the ICU or your hospital room.
You will move to a room in the hospital after staying in the ICU and your condition is stable. You will stay in the hospital for a few more days.
You may need oxygen for a while after surgery. Generally, the oxygen will be stopped before you go home.
You will be taught deep-breathing exercises. These will help to re-expand the lungs and prevent pneumonia.
Medical staff will check your brain function often and make sure your body systems are working correctly after surgery. To check your brain function, you will be asked to follow a variety of basic commands. These include moving your arms and legs. Your pupils will be checked with a flashlight, and you will be asked questions to assess your awareness. These might include your name, the date, and where you are. The staff will test the strength of your arms and legs.
The head of your bed may be raised to prevent swelling of your face and head. Some swelling is normal.
You will be encouraged to move around as you are able while in bed. As your strength improves, you will have help to get out of bed and walk around. A physical therapist (PT) may evaluate your strength, balance, and mobility. The PT will give you suggestions for exercises to do both in the hospital and at home.
You will likely have sequential compression devices (SCDs) placed on your legs while you are in bed to prevent blood clots. SCDs have an air compressor that slowly pumps air into and out of fitted sleeves that are placed on the legs. They help prevent blood clots by passively compressing the leg veins to keep blood moving.
You may be given liquids to drink a few hours after surgery. This depends on your case. Your diet may be slowly changed to include more solid foods, as you can handle them.
You may have a catheter in your bladder to drain your urine for a day or so, or until you are able to get out of bed and move around. Report any painful urination or other urinary symptoms that occur after the catheter is removed. These may be signs of an infection that can be treated.
You may be moved to a rehab facility for a while to regain your strength. This depends on your status.
Before you are discharged from the hospital, arrangements will be made for a follow-up visit with your healthcare provider. They will also give you instructions for home care.
At home
Once you are home, it is important to keep the incision clean and dry. Your healthcare provider will give you specific bathing instructions.
You may choose to wear a loose turban or hat over the incision. Don't wear a wig until the incision is completely healed (about 3 to 4 weeks after surgery).
The incision and your head may ache. This is especially true with deep breathing, coughing, and exertion. Take a pain reliever for soreness as advised by your healthcare provider. Aspirin or other blood-thinning medicines may increase the chance of bleeding. Be sure to take only advised medicines and ask if you are unsure.
Continue the breathing exercises used in the hospital to prevent lung infection. You will be advised to stay away from exposure to upper respiratory infections (colds and flu) and irritants. These include tobacco smoke, fumes, and environmental pollution.
Slowly increase your physical activity as tolerated. It may take a few weeks to return to your previous level of energy and strength.
You may be instructed to not lift heavy items for a few weeks to prevent strain on your surgical incision.
Don't drive until your healthcare provider says it's OK.
Get medical care right away if you have any of these symptoms:
-
Fever or chills
-
Redness, swelling, bleeding, or drainage from the incision site or face
-
Increased pain around the incision site
-
Vision changes
-
Confusion or excessive sleepiness
-
Weakness of your arms or legs
-
Speech problems
-
Trouble breathing, chest pain, anxiety, or change in mental status
-
Green, yellow, or blood-tinged sputum (phlegm)
-
Seizure activity
Your healthcare provider may give you other instructions about what to do after a craniotomy.
Next steps
Before you agree to the test or procedure make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how will you get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure